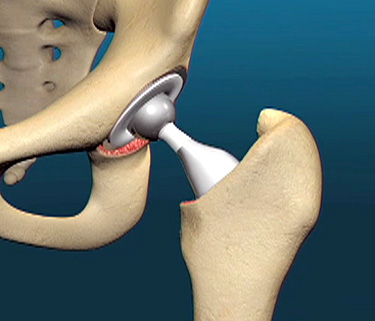
Total hip replacement is considered to be the most successful operation of the 20th century. It carries a success rate of 96-98 %. However there are some risks(although rare), which are infection(1%), deep vein thrombosis (normally blood does not clot with in our body, but following surgeries blood can clot within the blood vessels of the legs causing swelling of the legs. These clots could dislodge and the blood flow could carry them into the lungs(this is called pulmonary embolism). The other risks dislocation, leg length discrepancy, and anaesthetic complications.
The major complications of a hip replacement are:
- Dislocation: This is rare as the hip is a very stable joint; the incidence is <2%
2. Infections: This can be further classified as acute<2 weeks; intermediate upto 15 months and delayed anytime later.
Acute infections occur in the immediate post op period and may be because of contamination; seeding of bugs from another source. This may be managed with IV medications and local care like a lavage without removing the prosthesis.
Intermediate infections again are usually from seeding from other sites like teeth,lungs, kidneys etc. The management may be similar to the acute stage but not always can you save the prosthesis. This may require a staged revision if eradication of infection is the goal
Late infections like the term means infection at a late stage. This is usually secondary to other factors like infections of the urinary tract; pneumonia, and other systemic infection, which cause a septicemia and seeding of the organisms into the joint. These are generally handled with staged revisions namely removal and clean out of the joint; placement of an antibiotic spacer to maintain soft tissue tension/ architecture followed by a secondary joint placement. The success rate of these in the best of hands is about 75-80%
3. Deep vein thrombosis/phlebitis: This is blood clots forming in the leg veins. These can propagate and when they break off and end up in the lungs they can cause severe respiratory distress and even death. This is the reason for the calf compression device and or blood thinners used.
4. Respiratory problems like atelectasis/ pneumonia can happen. This is hopefully prevented with the chest compression exercises and deep breathing; you are encouraged to do coughing along with incentive spirometer
5. Prosthetic failure; Lysis Periprosthetic fractures: These though rare are seen with the longer duration the prosthesis is in place and can be due to wear; delamination of the polyethylene, cement failure with lysis. These are now to a certain extent managed with the advent of better bearings like ceramic and highly crosslinked polyethylene. Revisions in these cases can be difficult and would require specialized equipment as well as surgeons trained for this.
6. Loosening: There are 2 types of this problem, one caused by infection, when the organism creates /causes localized bone destruction and failure and the second due to aseptic causes which cannot be always identified. Mal alignment of the components especially of the stem can cause an abnormal dynamics which can increase wear and secondary failure.
7. Stem fracture: A very rare complication caused by improper cementing leading to distal fixation and cantilever bending.
8. Cup disassociation: very rare but can happen and is due to failure of the cup locking mechanism
9. Leg length discrepancy
What would be the type of anaesthesia used?
Most of the times a Spinal anaesthesia would be given but sometimes a general anaesthetic would also be used. The anaesthesiologist would evaluate and administer the most appropriate anaesthetic. The blood loss from this operation is about 300ml and usually does not require a transfusion.
When would I walk? what would happen during postoperative days in the hospital?
I or a colleague will see you later on the day after the hip replacement and get you up standing and may get you to take a few steps.
Physical therapy starts the same day or next and he works with you to start walking with a walker, manipulating stairs and also will go through the programme for you to use post discharge. Ambulation will be with a walker and we suggest this for the first 3-4 weeks.We will make arrangements for a bed side commode for use in the hospital and suggest you modify your toilet at home so as to raise the seat. We do not want you to bend your hip more than 90 degrees. It is advisable to always have a pillow between your legs so that you don’t cross your legs. Try and keep the foot and knee looking straight up when lying in bed.
The dressings are changed prior to discharge and we do not want you to fool with it, till we see you in the clinic.You should avoid getting your wound wet till we see you in the clinic and so you will skip showers/bath and just sponge/towel baths.
Deep breathing, coughing will also be encouraged as well as the use of the spirometer. This is done to get your lungs to expand fully.
I generally let you go home the third or fourth day.